Opioid Addiction: Understanding Causes and Effective Paths to Recovery
Opioid Use Disorder (OUD) is a chronic medical condition characterized by compulsive opioid use despite harmful consequences, and it affects individuals across ages and communities. This article explains the biological, psychological, and social drivers of opioid addiction, outlines observable signs and common stages, reviews how the opioid crisis has evolved through three distinct waves, and summarizes evidence-based treatment and recovery strategies. Readers will gain clear guidance on early recognition, the role of medication-assisted treatment (MAT) — including methadone, buprenorphine, and naltrexone — and how behavioral therapies support lasting recovery. The guide also presents recent 2022–2024 trends and practical steps for families and communities to reduce stigma and improve outcomes. Because no specific provider is referenced, the focus remains general and evidence-oriented, drawing on contemporary public-health framing and clinical consensus. Throughout, common terms like naloxone, fentanyl, overdose prevention, and harm reduction are used to connect clinical concepts to practical actions.
What Are the Causes and Risk Factors of Opioid Addiction?
Opioid addiction arises from an interaction of exposure, neurobiology, and environment: opioid exposure initiates reward-circuit reinforcement, genetic and neuroadaptive factors alter vulnerability, and social or situational risks increase the chance of escalation. Understanding these mechanisms clarifies why some people progress from prescribed short-term use to dependence while others do not, and it points to prevention strategies such as safer prescribing and early screening. Below is a concise list of primary causes and risk factors to aid rapid recognition and early intervention. The list highlights proximal drivers that clinicians, families, and policymakers can address to reduce incidence and harm.
This section summarizes the most common causes of opioid addiction:
- Prescription opioid exposure: Initial medical prescriptions for pain can create tolerance and craving that lead to long-term use.
- Genetic vulnerability: Family history and heritable traits increase risk by shaping reward and stress-response systems.
- Chronic pain and inadequate pain management: Persistent pain often leads to escalating doses and prolonged opioid exposure.
- Trauma and mental health conditions: PTSD, depression, and anxiety increase self-medication behaviors with opioids.
- Social and economic factors: Unemployment, peer drug use, and high local opioid availability raise initiation and relapse risk.
These causes interact: prescription exposure + pain + psychosocial stressors often combine to produce opioid use disorder, which implies prevention must be multifaceted. Recognizing these drivers supports targeted actions such as screening for ACEs, using multimodal pain care, and implementing safer-prescribing protocols that reduce new cases of OUD.
How Do Genetic and Environmental Factors Contribute to Opioid Use Disorder?

Genetic predisposition influences susceptibility to opioid addiction by altering neurotransmitter systems, reward sensitivity, and impulsivity, which together modulate risk when drugs are introduced. Twin and family studies indicate a meaningful heritability component, while gene-environment interactions show that genetic risk is often triggered or amplified by life stressors and adverse childhood experiences. Environmental factors such as peer substance use, community drug supply, and socioeconomic instability create exposure pathways and normalize opioid use, increasing the probability of escalation.
Clinically, this means screening for family history and ACEs helps identify higher-risk patients and informs early prevention measures like close follow-up and referral to behavioral health supports.
What Role Do Chronic Pain and Emotional Distress Play in Developing Addiction?
Chronic pain creates prolonged opioid exposure through repeated prescribing and dose escalation, fostering tolerance and physiologic dependence that can progress to misuse and addiction. Emotional distress and untreated mental illness frequently co-occur with chronic pain; individuals may use opioids to self-medicate negative affect, which reinforces substance-related coping patterns and complicates recovery.
Safer pain management emphasizes multimodal therapy—physical rehabilitation, non-opioid analgesics, interventional approaches, and psychological treatments—to reduce reliance on long-term opioids. For patients on chronic opioid therapy, routine screening for OUD symptoms, mental-health comorbidity, and early referral to addiction specialists are essential prevention steps.
| Risk Factor | Mechanism | Prevention / Mitigation |
|---|---|---|
| Prescription exposure | Initiates reward-circuit reinforcement and tolerance | Implement guideline-based prescribing, shortest effective duration, and prescription monitoring |
| Genetic vulnerability | Alters reward and stress pathways increasing susceptibility | Screen family history; provide early education and monitoring |
| Chronic pain | Long-term exposure leads to dose escalation and dependence | Use multimodal pain management and reassess opioid efficacy regularly |
This table maps causes to mechanisms and concrete prevention measures that clinicians and policymakers can adopt to reduce development of opioid use disorder.
What Are the Signs and Stages of Opioid Addiction?
Opioid addiction manifests across behavioral, physical, and functional domains: early signs include mood changes and doctor-shopping, while later stages show marked decline in occupational or social functioning and compulsive drug seeking despite harm. Clinicians and families should focus on observable changes in daily behavior, increasing tolerance, withdrawal symptoms, and loss of control as red flags prompting assessment. Below is a four-stage model that clarifies progression and actionable responses at each stage. Recognizing stage-appropriate interventions improves the chance of early treatment and reduces overdose risk.
The progression of opioid addiction typically follows four stages:
- Initiation: Use begins, often via prescription or experimentation, with occasional use and perceived control.
- Escalation: Frequency and dose increase as tolerance builds; use becomes more regular and risky.
- Dependence: Physiologic dependence is evident through withdrawal symptoms when use stops.
- Addiction/Entrenchment: Compulsive drug-seeking and loss of control dominate behavior despite negative consequences.
These stages serve as a practical framework: early-stage identification enables brief interventions or medication-assisted treatment initiation, whereas later stages commonly require intensive treatment and comprehensive relapse-prevention planning.
What Are the Four Stages of Opioid Addiction?
The four-stage model—initiation, escalation, dependence, and addiction—describes a typical path from first exposure to entrenched disorder, each with characteristic behaviors and intervention opportunities. Initiation often follows a medical prescription or social exposure; clinicians can reduce risk by limiting prescriptions and educating patients. During escalation, signs such as dose increases, lost prescriptions, or risky procurement should prompt assessment and linkage to treatment. In dependence and addiction stages, evidence supports initiating medication-assisted treatment, managing withdrawal safely, and combining behavioral therapies to restore function and reduce overdose risk.
How Can You Recognize Early Symptoms of Opioid Use Disorder?
Early symptoms include increased tolerance, withdrawal signs (nausea, agitation), social withdrawal, decreased performance at work or school, and changes in sleep or mood that differ from prior baseline. Simple screening prompts for family members and clinicians include asking about changes in prescription use, unexplained mood shifts, frequent requests for refills, or evidence of obtaining opioids from multiple providers.
When these red flags appear, immediate safety steps include assessing overdose risk, ensuring naloxone availability, and arranging a clinical evaluation for OUD. Early recognition paired with timely intervention can significantly improve outcomes and reduce progression to severe addiction.
How Has the Opioid Crisis Evolved and What Are the Latest Statistics?
The opioid crisis has unfolded in three waves: the rise of prescription opioid-related harms, a shift to heroin, and the current surge of synthetic opioids dominated by fentanyl; each wave reflects changes in availability, prescribing, and illicit market dynamics. Recent trends through 2022–2024 emphasize the dominance of synthetic opioids in overdose fatalities and the increasing complexity of polysubstance involvement, especially stimulants combined with fentanyl. Understanding these waves clarifies where prevention, harm reduction, and treatment investments should be targeted.
The compact table below summarizes key metrics to inform policymakers, clinicians, and community stakeholders.
| Metric | Year / Trend | Value & Interpretation |
|---|---|---|
| Overdose deaths (US) | 2022–2024 trend | Continued high-level mortality with synthetic opioids driving most increases; surveillance shows regional variation |
| Share involving synthetic opioids | 2022–2024 trend | Majority proportion of opioid-involved deaths now involve fentanyl or analogs, indicating potency-driven risk |
| Treatment gap (% with OUD receiving MAT) | Recent estimate trend | Substantial treatment gap persists, with many individuals not receiving FDA-approved medications despite evidence of benefit |
What Are the Three Waves of the Opioid Epidemic?
The three-wave framework captures shifts in the primary drivers of opioid mortality and service needs: the first wave (prescription opioids) arose from expanding medical opioid use, the second wave reflected increasing heroin availability and use as prescription supply was restricted, and the third wave began with the infiltration of illicitly manufactured fentanyl and powerful analogs that markedly increased overdose risk. Each transition involved market adaptations and policy responses, and each wave demanded different public-health strategies—safer prescribing for wave one, expanded addiction treatment for wave two, and aggressive harm reduction and naloxone distribution for wave three. Understanding this history aids targeted interventions at the community and clinical levels.
What Do 2022-2024 Opioid Overdose Statistics Reveal?
Recent data from 2022–2024 show that synthetic opioids account for a large and growing share of opioid-involved overdose deaths, while stimulant co-involvement has also risen, complicating prevention and treatment strategies. Overdose counts remain elevated in many regions despite localized declines, signaling persistent supply-side potency and access issues as drivers. Treatment access metrics reveal that a notable portion of people with OUD still do not receive MAT, indicating ongoing system barriers such as regulatory limits, workforce shortages, and stigma. These statistical patterns underscore the need for scalable harm-reduction services, expanded MAT availability, and comprehensive public-health responses.
| Metric | Year / Trend | Value & Short Interpretation |
|---|---|---|
| Synthetic opioid proportion | 2022–2024 | Majority of opioid deaths; potency increases overdose risk rapidly |
| Polysubstance involvement | 2022–2024 | Rising co-use with stimulants complicates clinical management |
| MAT coverage | 2022–2024 | Persistent treatment gap underscores need for expanded access |
What Are the Most Effective Treatment Options for Opioid Use Disorder?
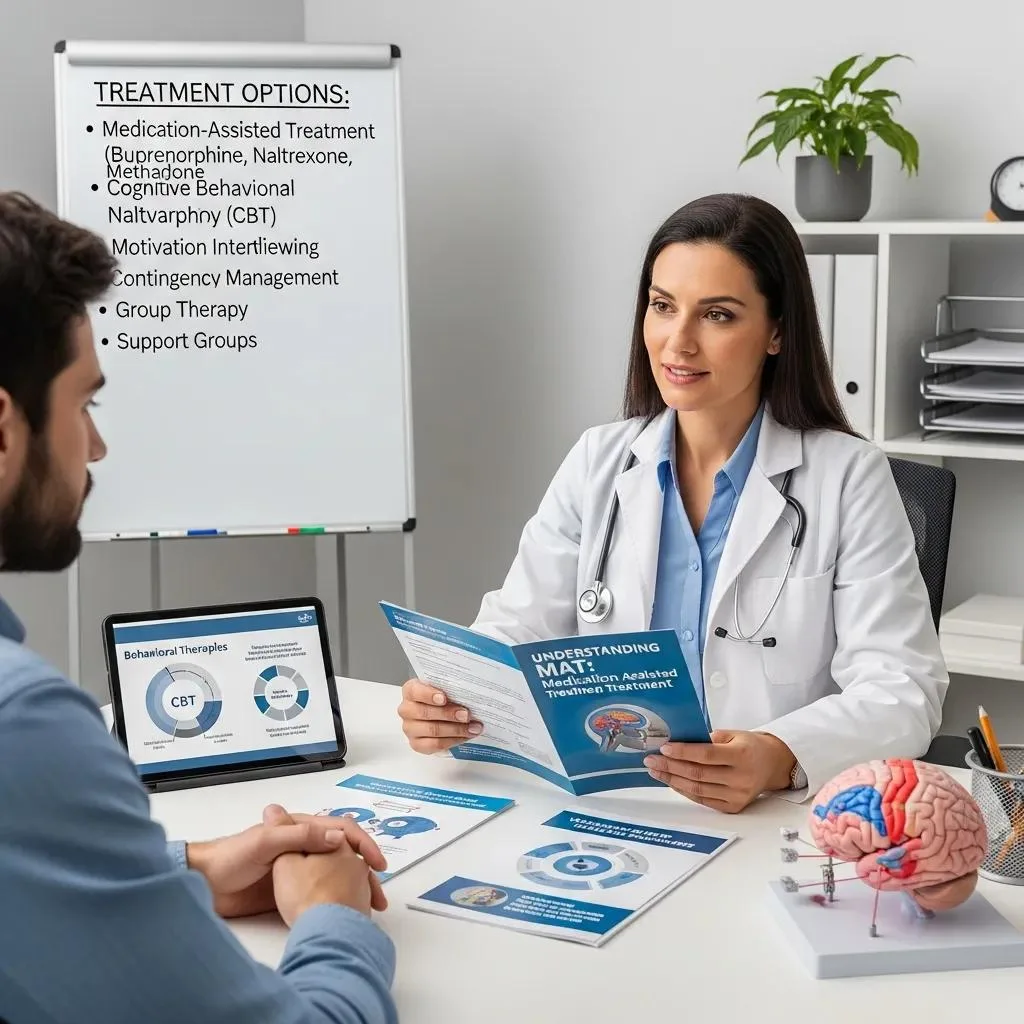
Effective treatment for OUD combines medication-assisted treatment (MAT) with behavioral therapies and appropriate levels of care; MAT with methadone, buprenorphine, or naltrexone reduces withdrawal, cravings, and overdose risk while behavioral therapies address relapse triggers and coping skills. Selection of medication and level of care depends on clinical presentation, patient preference, and local availability, with evidence favoring retention on methadone or buprenorphine for improving outcomes. The comparison table below summarizes key medications and therapies to help clinicians and patients evaluate options quickly and accurately. Integrating pharmacologic and psychosocial care produces the best chances for sustained recovery and reduced mortality.
| Medication / Therapy | Mechanism / Setting / Typical Duration | Pros & Cons |
|---|---|---|
| Methadone | Full opioid agonist; clinic-based dosing; long-term maintenance often months to years | High retention; reduces overdose risk; clinic access limits can be barrier |
| Buprenorphine (Suboxone/Subutex) | Partial agonist; office-based or telehealth initiation; maintenance months–years | Flexible access; lower overdose risk; prescriber waiver requirements have been relaxed in the US but may vary by region |
| Naltrexone (Vivitrol) | Opioid antagonist; requires detox before start; monthly injection option | Blocks opioid effects; adherence challenges; not suitable for those unable to complete detox |
| CBT / MET / Contingency management | Behavioral interventions in outpatient/residential settings; duration varies | Improves coping, reduces relapse; best combined with MAT for opioid use disorder |
How Does Medication-Assisted Treatment Work?
Medication-assisted treatment uses medications to stabilize brain chemistry, reduce cravings, and prevent withdrawal, which allows patients to engage more fully in behavioral therapy, recovery planning, and social reintegration. Methadone acts as a long-acting opioid agonist that prevents withdrawal and decreases illicit opioid use; buprenorphine’s partial agonist activity provides safety and flexibility in many treatment settings, and naltrexone blocks opioid receptors to prevent intoxication. Benefits of MAT include improved retention in care, reduced mortality, and decreased criminal activity and infectious-disease risk, while limitations involve access barriers, regulatory constraints, and adherence challenges. Overcoming these barriers through expanded prescribing, low-threshold programs, and integrated behavioral supports increases population-level impact.
What Behavioral Therapies Support Long-Term Recovery?
Behavioral therapies such as Cognitive Behavioral Therapy (CBT), Motivational Enhancement Therapy (MET), contingency management, and trauma-informed family therapy address maladaptive behaviors, motivation, and environmental triggers that contribute to relapse. CBT provides skills to identify and change thought patterns that lead to substance use, MET enhances readiness for change, and contingency management uses tangible incentives to reinforce abstinence. Family- and trauma-informed approaches address underlying relational and traumatic drivers, improving engagement and long-term functioning. Combining these therapies with MAT produces superior outcomes compared to medication alone by targeting both biological and psychosocial dimensions of opioid addiction.
| Treatment Option | Setting | Key Benefit |
|---|---|---|
| Methadone | Opioid treatment program | High retention and overdose reduction |
| Buprenorphine | Office/telehealth | Greater accessibility; flexible maintenance |
| CBT / MET | Outpatient/residential | Skills-building and motivation enhancement |
This concise table reinforces the complementarity of medications and behavioral interventions in effective OUD care.
How Can Individuals Sustain Recovery and Overcome Stigma?
Sustaining recovery requires ongoing relapse-prevention planning, engagement with peer support, access to long-term follow-up care, and strategies that reduce stigma and social isolation. Practical steps include developing coping skills for cravings, maintaining medication adherence where indicated, participating in peer groups or mutual-aid programs, and ensuring family supports and contingency planning for triggers.
- Relapse-prevention planning: Establish coping plans for triggers, high-risk situations, and medication contingencies.
- Peer support engagement: Participate in peer recovery groups or trained recovery coaching to enhance retention.
- Family involvement and education: Use nonjudgmental communication, set boundaries, and learn overdose response.
- Community harm reduction: Support naloxone availability, syringe services, and treatment access advocacy.
Implementing these steps together—individual planning, peer supports, family engagement, and community-level harm reduction—creates a comprehensive recovery ecosystem that reduces relapse risk and counters stigma.
What Role Do Peer Support and 12-Step Programs Play in Recovery?
Peer support and mutual-aid groups provide social connectedness, accountability, and practical recovery skills that often complement formal clinical treatment, enhancing retention and reducing isolation. Evidence suggests that peer-based services and 12-step participation can improve treatment engagement and support long-term abstinence for many individuals when integrated with MAT and counseling. Different models—peer recovery specialists, SMART Recovery, 12-step fellowships—offer varying emphases on spirituality, skills training, or peer coaching, allowing patients to choose fits for personal values and needs. Limitations include variable structure and availability; linking peer support with professional care maximizes benefits.
How Can Families and Communities Help Reduce Stigma Around Opioid Addiction?
Families and communities reduce stigma by adopting person-first language, educating about OUD as a treatable medical condition, and supporting policies that expand treatment and harm-reduction services. Practical family steps include listening without blame, setting boundaries that protect safety, learning overdose response (naloxone use), and encouraging engagement with evidence-based treatment. Workplaces and community organizations can implement supportive policies, employee assistance, and public education campaigns to change public perceptions and increase access to care. Collective action—combining education, policy change, and visible support for recovery—creates environments where individuals are more likely to seek help and sustain recovery.
| Community Action | Purpose | Expected Impact |
|---|---|---|
| Naloxone distribution | Overdose reversal | Immediate reduction in fatal overdoses |
| Public education campaigns | Reduce stigma | Increased treatment-seeking and community support |
| Expanded MAT access | Treatment availability | Lower mortality and improved recovery rates |
This final table encapsulates community-level interventions that meaningfully reduce harm and support recovery across populations.




